By Ghadeer Ghloum
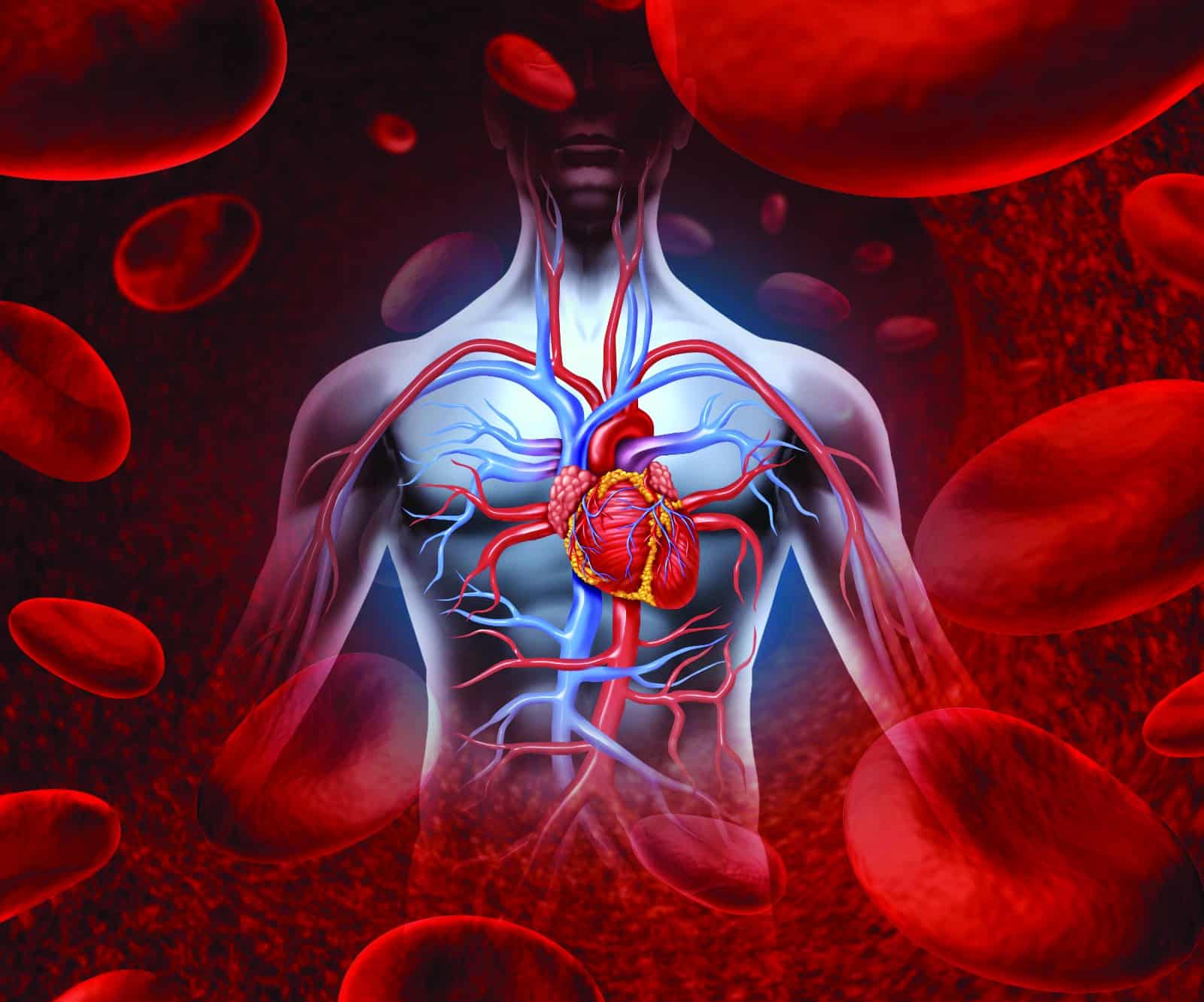
KUWAIT: Kuwait Times delved into the differences in cardiovascular health between males and females and sudden heart failure among people, including youth, during an interview with Dr Abdullah Esmaiel, Canadian and American board certified doctor in cardiology and interventional and structural catheterization.
Kuwait Times: Are there any differences in the prevalence of coronary artery disease between men and women?
 Dr Abdullah Esmaiel
Dr Abdullah EsmaielDr Abdullah Esmaiel: Coronary artery disease (CAD) is not just a “man’s disease”, and its effect on women tends to be riddled with misunderstandings. Women are just as likely as men to develop CAD; however, in women, CAD usually develops seven to 10 years later in life compared to men. Menopause seems to trigger a host of risk factors, including weight gain, higher blood pressure and unfavorable changes in cholesterol levels.
KT: Are there differences in the symptoms experienced by men and women during a heart attack?
Dr Esmaiel: Chest pain or discomfort is the most common symptom of a heart attack for both men and women. However, women are more likely than men to have additional symptoms as well, such as nausea and shortness of breath. Chest pain can take various forms, such as chest pressure, tightness, squeezing or burning, discomfort in your chest, shoulders, arms, back or jaw, pain that travels down one or both arms and shortness of breath. Other symptoms include unusual or extreme tiredness, feeling dizzy or lightheaded, nausea or vomiting, cold sweat and anxiety.
KT: Are there disparities in cardiovascular outcome based on gender?
Dr Esmaiel: Women tend to have poorer cardiovascular outcomes than men due to a multitude of factors, including underuse of evidence-based medical therapies, delays in presentation, diagnosis and treatment, and lack of gender-specific data regarding the appropriate treatment of coronary artery disease in women.
KT: Are there variations in the risk factors for heart disease between genders?
Dr Esmaiel: Traditional risk factors for heart disease and stroke are similar in men and women; this includes smoking, having high blood pressure, high cholesterol or diabetes, not exercising routinely or sitting for long periods of time, eating a diet high in processed foods, salt, saturated fats, cholesterol and added sugars, being overweight or obese, family history of early heart disease and older age. Race, such as being black or South Asian is also linked with a higher risk.
Diabetes, mental stress or depression, obesity and smoking tend to play a bigger role in the development of CAD in women when compared to men. Heart disease can happen at any age, but it tends to increase in women around or after menopause. Other female-specific risks known to increase the likelihood of heart disease include having started menstruating before 10 or after 17 years of age, having health problems during pregnancy, such as hypertensive disorders or gestational diabetes during pregnancy, preterm delivery, polycystic ovarian syndrome (many ovarian cysts) and oral birth control.
It is also a concern if you smoke, have spontaneous coronary artery dissection (SCAD) or autoimmune diseases such as lupus (SLE) or rheumatoid arthritis (RA).
KT: Are there any gender-specific preventive measures or interventions that can be taken to reduce the risk of heart disease?
Dr Esmaiel: Protecting the heart by controlling the risk factors, ie, hypertension, diabetes or high cholesterol. Adopting heart-healthy habits, such as exercising, eating right, getting enough rest and not smoking, is equally important in men and women. However, what is specific for women is that they are natural caretakers. Whether she is as a mother, sister, daughter or wife, women are often so busy caring for everyone else that their health and well-being slip to the bottom of the list. So, remember to take care of your health to be able to take care of others.
KT: What is sudden arrhythmic death syndrome (SADS) that causes sudden death in youngsters? Are there any symptoms that can alert us to SADS?
Dr Esmaiel: Sudden arrhythmic death syndrome is when someone dies suddenly and unexpectedly from a cardiac arrest, but the cause of the cardiac arrest cannot be found. A cardiac arrest is when your heart suddenly stops pumping blood around your body. SADS usually happens when an abnormal heart rhythm leads to cardiac arrest. It is usually caused by a heart condition that affects the heart’s electrical system — these conditions are caused by changes in one or more of our genes. Unfortunately, most of these conditions have no “alarming signs or symptoms”. The most important thing to do is to seek medical advice regarding screening and genetic testing if you have a relative who suffered from SADS to prevent another event in the family.